680
Views & Citations10
Likes & Shares
Background: The aim of
this study is to evaluate the comparative effects of the diode lasers in animal
models. Many surgical instruments like scalpel, electrosurgery and different
laser types can be used for surgical incisions. Each of these has their own
advantages and disadvantages.
Methods: Dorsal skin
incisions, 10 mm in length and 1 mm in depth, were created on male Wistar
albino rats via 3 different laser wavelengths. The animals were sacrificed at
post-operative 24 h, 3 days or 1 week. All incision sites were removed by
excisional biopsies and the specimens underwent histological examination.
Results: There were no
statistically significant differences in the thermal changes, inflammation
levels and fibrosis in all wavelength groups (p>0.05).
Conclusion: Pulsed mode
of lasers accelerates the epithelisation regardless of the wavelengths.
Keywords: Diode
lasers, Wound healing, Continuous wave lasers, Pulsed lasers
INTRODUCTION
Wound healing is divided into four topics as coagulation, inflammation,
proliferation and maturation. The main events occurred during the healing are
angiogenesis, epithelisation, granulation tissue formation and collagen
deposition in the proliferation phase [1-3].
Numerous surgical instruments have been introduced in dental practice
for surgical purpose. These include scalpel, electrosurgery, CO2,
Nd:YAG, Er:YAG and diode lasers. Each of these devices has their own advantages
and disadvantages. Steel scalpel also known as cold knife has been commonly
preferred for
many
Electrosurgery
is a surgical process that uses high frequency electrical currents [7].
Electrosurgery provides adequate hemostasis by sealing the vessels before
cutting. On the other hand, wound healing is delayed by extensive thermal
injury and also electrosurgery units have the disadvantage of causing muscle
fasciculation [5-8].
The use of soft
tissue lasers for the surgical procedures in dentistry aims to provide benefits
to both the dentist and the patient [7,9]. Medical and dental researchers began
to study different type of laser for intraoral surgical procedures. Diode
lasers are the most common laser type owing to its compact size affordability
and possibility to be used in in many applications such as endodontics, soft
tissue surgery, periodontics, orthodontics, bleaching and low level laser
therapy (LLLT). It was introduced in mid-90 by Harris and Pick in 1995. Latest
reports have suggested that diode laser with wavelengths between 810 to 970 nm
in continuous and pulsed mode is a possible equipment for soft tissue surgery
in the oral region [5,9]. Furthermore, diode lasers have a fiber optic tip that
provides opportunity to work with or without contact depending on the clinical
requirements. Great absorption in hemoglobin with result of giving a good
bleeding control is another reason of this choice. This feature provides
bloodless area and clear view of the operative field and also there is often no
need for a suture after the incision [4,10,11]. Heat produced during laser
incision causes protein denaturation, drying, vaporization and carbonization of
the application area. As a result of that pain, receptors at the incision area
are inhibited. This eliminates the necessity of anesthetics injection and
disinfection of the field. A better and faster healing process provides a good
comfort to the patient after the operation so no medication is needed [7,12].
There are
different wavelengths of diode lasers that were produced by various companies
in the market and each diode laser has continuous and pulsative application
mode. It has a crucial importance to determine the soft tissue damage resulting
from standardized incision using different wavelengths and application modes
[8,13]. However, no studies have assessed the effectiveness of each diode laser
and the efficiency of the mode of application as pulsative or continuous.
Therefore, this study aims to evaluate the comparative effects of the diode
lasers of 3 different wavelengths in animal models. The first null
hypothesis of the study is that there is no effect of the wavelength and the
second one is that there is no effect of mode of application on the wound
healing in animal models.
MATERIALS AND METHODS
Male
Wistar albino rats with a weight of 250-300 g body mass and 5 months old were
used in the study. Ethical clearance was taken from Committee on Animal
Research of Bezmialem Vakif University (Protocol number: 2015/243). The rats
were anesthetized by intramuscular injection of ketamine 35 mg/kg and xylazine
HCL 5 mg/kg. Following anesthesia, the dorsum (operative field) of each rat was
shaved with an electric shaver. After marking the incision line on every rat, 3
different laser wavelengths; 810 nm (Gigaa, Cheese, China), 940 nm (Epic 10,
Biolase, USA) and 980 nm (SIROlaser Advance, Sirona, Bensheim, Germany) were
used to create an incision (10 mm in length and 1 mm in depth) on animals’
dorsal side to the subcutaneous level using the lasers in continuous (3 W/cm2)
or chopped modes (3 W/cm2 50% Duty cycle). Totally each rat had 6
incisions that were cut at least 1 cm apart.
The animals
were sacrificed after 24 h, 3 days or 1 week. Incision areas of the dorsal side
of each rat were removed by excisional biopsy and the specimens underwent
histological examination. The specimens were fixed in formalin (10%) processed
in the usual manner and embedded in paraffin blocks. They were sectioned and
stained with standard hematoxylin and eosin solution. Light microscope (CX 31;
Olympus, Tokyo, Japan.) was used for histological examination. Sections were
evaluated by a pathologist and thermal changes, closure of epithelium
granulation tissue, inflammation and fibrosis were recorded (grading range 0 to
3+).
Statistical
analysis was executed with Statistical Package for Social Science (SPSS v.22.
Chicago.IL, USA) for Windows 10.0 and where appropriate Kruskal Wallis and Mann
Whitney U tests were for pairwise comparisons among groups (a=0.05).
RESULTS
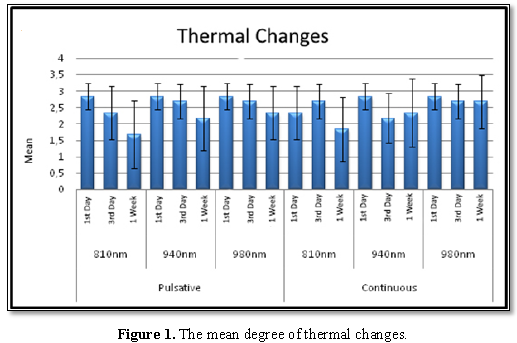
Figure 1 shows the thermal
changes on the tissues after laser irradiations groups. There were gradually
decrease day by day in all wavelengths and application modes; however, there
were no statistically differences among the tested days (p>0.05).
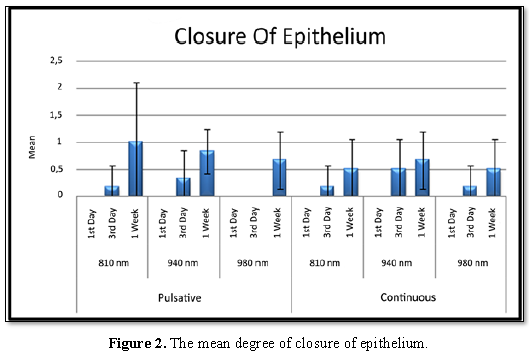
After bilateral comparisons
to determine the days of significance; the level of epithelial closure in the
seventh day was found significantly higher on the first day in all wavelength
groups (p<0.05). There was no significant difference between epithelial
closure grades on the first day and on the third day in all wavelength groups
(p>0.05) (Figure 2).
DISCUSSION
In dentistry,
the used wavelengths of the diode lasers are 655, 810, 940, 1064 nm,
respectively [14]. They are used for different clinical applications such as
cutting/destructing tissues and coagulating bleeding. 810, 940 and 980 nm
wavelengths are ideal for soft tissue applications due to the well absorption
characteristics by melanin and hemoglobin with a penetration depth between 0.5
to 3 mm. Not only the wavelength but the power, pulse duration, fiber diameter
and frequency may also affect the cutting efficiency of lasers on the soft
tissues. Thermal damage of the tissue may be influenced by the following
factors: output power, wavelength, affinity with the target tissue, terms
transmission and type of the optical fiber [14]. Yammie et al. [14] investigated
diode lasers with three different wavelengths 810, 940, 980 nm similar to our
study. They have created 10 incisions measuring 10 mm in length and 2 mm in
depth on fourteen male rabbits’ ventral surface of their tongues. The laser
parameters were 2 W with continuous mode delivered using a 400 nm optical
fiber. They have detected similar thermal denaturation such as carbonization in
different wavelength groups. They have reported that there was no statistically
significant difference for the cutting depth and the incision’s width. They
have observed that 940 nm groups showed a wider marked carbonization zone but
there was no statistically significant difference between the groups. The
highest necrotic zone reported at 980 nm group but there was no statistically
significant difference, either. They also reported no significant difference
for inflammatory zones among the groups [14]. Similar to Yammie et al.’s [14]
study, our results showed no statistically significant difference of the
different wavelengths for the inflammatory zones; we also found no
statistically significant difference between chopped and continuous modes.
Jin et al. [15]
investigated guinea pig mucosa wound healing on the 15 mm length incisions
created by a scalpel, diode laser and Er, Cr:YSGG laser. The laser used in this
study is 810 nm diode lasers with 2 W of power, pulse length of 0.5 ms
continuous wave and aiming beam of 635 nm. They used continuous mode and with
non-contact technique. The inflammatory response at diode laser group had the
lowest values at post surgery of the first day but at postsurgical 3 and 5 day
groups the inflammation at the diode laser group was the highest [15]. They
also investigated TNF-α and TNF-β1 expression in the groups and concluded that
diode laser was a good device for oral mucosal incisions but the tissue damage
created by diode laser was higher than the scalpel or Er, Cr:YSGG laser. Kaur
et al. [16] investigated two different techniques as scalpel and diode laser
(810 nm) for uncovering the implants, found no statistical significant
difference between healing index scores.
Saperia et
al.’s [17] research which was the first study to evaluate the effect of laser
on wound healing using the technique of molecular biology, they made
whole-layer wounds in the back of pig and created three different groups as
irradiation with Helium-Neon laser, tungsten light and no light each other. In
laser and tungsten groups, Types I and III procollagen mRNAs were expressed
more than in non-irradiation group. They proposed that laser irradiation
increased collagen synthesis [17].
Suzuki et al.
[18] investigated the wound healing efficacy of a 660 nm diode laser with
different energy densities in a rat incisional wound model. Samples were
divided into groups to receive 660 nm diode laser irradiation 24 h after
surgery at an energy density of 0 (control), 1, 5 or 10 J/cm2.
Tissue sections were stained with hematoxylin-eosin and an antibody for ED1 to
determine the number of macrophages around the wound. They found that 660 nm
diode laser with energy density of 1 and 5 J/cm2 enhanced wound
healing in a rat incisional wound whereas increased laser irradiation failed to
yield such enhancement.
Mun et al. [19]
have performed an animal study to clarify the effect of diode laser on wound
healing based on microscopic findings. Laser diode of 655, 785 and 850 nm
wavelengths were irradiated to the rat skin wound for 9 days, 20 min a day.
They concluded that group of 850 nm resulted in the most abundant collagen
formation so diode laser had beneficial effects on the formation of fibroblast
and collagen and resulted in better wound healing. In our study, there was no
statistically significant difference in the fibrosis between first, third and
seventh days for three wavelength when pulsed and continuous mode were used.
This result may come from that the method difference. Saperia et al. [17] and
Mun et al. [19] and Suzuki et al. [18] did not create the wounds with laser,
they just apply laser after the wound created to assess the healing properties.
There are many studies assessing the healing effects of different kind of
lasers on wounds/scars, but the studies assessing healing of wounds created by
lasers are limited.
Paysse et al.
[20] compared structural and functional outcomes and efficiency of diode laser
photocoagulation for retinopathy of prematurity (ROP) when delivered in a
pulsed mode versus a near-continuous mode. They concluded that there were no
differences at functional outcome, complications, structural outcome found
between using pulsed and near-continuous mode diode laser delivery for
high-risk ROP.
Bryant et al.
[21] compared the incisional wound healing created by scalped and CO2
laser on canine oral mucosa and monitored at 3, 7, 14 days after the incision,
they found a significant delay in the laser group and they linked the situation
to excess thermal damage of the continuous wave laser beam. They also reported
that short pulsed-free electron laser caused by the delay from the scalpel
group on wound healing shortens. They concluded that the importance of laser
pulse duration was much more important on the wound healing than the
wavelength. Our study’s results which are compatible with Bryant et al.’s [21]
findings, chopped mode laser applications and showed faster epithelization than
the continuous mode independent from the wavelength.
Havel et al. [22] compared 940 nm and 1470 nm wavelength laser diode system in vitro and in vivo. In vitro setup was on porcine liver and turkey muscle tissue model and for in vivo evaluation, 20 patients with nasal obstruction due to hyperplasia of inferior nasal turbinates were included in trial. They reported that the healing process following non-contact diode laser application revealed to be improved using 1470 nm diode laser compared to 940 nm. In our study, 940 nm and 810 nm continuous mode applications show faster granulation tissue formation.
CONCLUSION
Within the
limitation of this study, the chopped mode of lasers accelerates the
epithelisation regardless of wavelengths.
CONFLICT OF INTEREST
The authors declare
that they have no conflict of interest.
FUNDING
This research
did not receive any specific grant from funding agencies in the public,
commercial or not-for-profit sectors.
1. Singer AJ, Mach C, Thode HC Jr, Hemachandra S,
Shofer FS, et al. (2000) Patient priorities with traumatic lacerations. Am J
Emerg Med 18: 683-686.
2. Bock O, Schmid-Ott G, Malewski P, Mrowietz U (2006)
Quality of life of patients with keloid and hypertrophic scarring. Arch
Dermatol Res 297: 433-438.
3. Gunay A, Atilgan S, Yesilova Y, Yaman F, Ozgoz M,
et al. (2012) A comparative evaluation of the effects of bevacizumab and
5-fluorouracil on wound healing in rat model. HEALTHMED 6: 3937-3945.
4. D'Arcangelo C, Di Nardo Di Maio F, Prosperi GD,
Conte E, Baldi M (2007) A preliminary study of healing of diode laser versus
scalpel incisions in rat oral tissue: A comparison of clinical, histological
and immunohistochemical results. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod 103: 764-773.
5. Amaral MB, de Avila JM, Abreu MH, Mesquita RA
(2015) Diode laser surgery versus scalpel surgery in the treatment of fibrous
hyperplasia: A randomized clinical trial. Int J Oral Maxillofac Surg 44:
1383-1389.
6. Figurova M, Ledecky V, Karasova M, Hluchy M,
Trbolova A, et al. (2016) Histological Assessment of a combined low-level
laser/light-emitting diode therapy (685 nm/470 nm) for sutured skin incisions
in a porcine model: A short report. Photomed Laser Surg 34: 53-55.
7. Bhatsange A, Meshram EP, Waghamare A, Shiggaon L,
Mehetre V (2016) A clinical and histological comparison of mucosal incisions
produced by scalpel, electrocautery and diode laser: A pilot study. J Dent
Lasers 10: 37-42.
8. Goharkhay K, Moritz A, Wilder-Smith P, Schoop U,
Kluger W, et al. (1999) Effects on oral soft tissue produced by a diode laser
in vitro. Lasers Surg Med 25: 401-46.
9. Azevedo AS, Monteiro LS, Ferreira F, Delgado ML,
Garcês F, et al (2016) In vitro histological evaluation of the surgical margins
made by different laser wavelengths in tongue tissues. J Clin Exp Dent 8: e388-e396.
10. Fornaini C, Merigo E, Sozzi M, Rocca JP, Poli F, et
al. (2016) Four different diode lasers comparison on soft tissues surgery: A
preliminary ex vivo study. Laser Ther 25: 105-114.
11. Angiero F, Benedicenti S, Romanos GE, Crippa R
(2016). Treatment of hemangioma of the head and neck with diode laser and
forced dehydration with induced photocoagulation. Photomed Laser Surg 26:
113-118.
12. Laçin N, Kaya B, Deveci E, Kadiroğlu ET, Aktaş A,
et al. (2018) Comparative evaluation of ozone treatment in critical size bone
defects reconstructed with alloplastic bone grafts. Int J Clin Med 9: 566-579.
13. David CM, Gupta P (2015) Lasers in dentistry: A
review. Int J Adv Health Sci 2: 7-13.
14. Yammine S, Jabbour E, El Toum S, Cassia A (2018)
Histological study of induced incisions on rabbits' tongues with three diode
lasers with different wavelengths in continuous mode. Scientifica (Cairo) 2018:
2691942.
15. Jin JY, Lee SH, Yoon HJ (2010) A comparative study
of wound healing following incision with a scalpel, diode laser or Er, Cr:YSGG
laser in guinea pig oral mucosa: A histological and immunohistochemical
analysis. Acta Odontol Scand 68: 232-238.
16. Kaur M, Sharma YPD, Singh P, Sharma S, Wahi A
(2018) Comparative evaluation of efficacy and soft tissue wound healing using
diode laser (810 nm) versus conventional scalpel technique for second-stage
implant surgery. J Indian Soc Periodontol 22: 228-234.
17. Saperia D, Glassberg E, Lyons RF, Abergel RP,
Baneux P, et al. (1986) Demonstration of elevated type I and type III
procollagen mRNA levels in cutaneous wounds treated with helium-neon laser.
Proposed mechanism for enhanced wound healing. Biochem Biophys Res Commun 138:
1123-1128.
18. Suzuki R, Takakuda K (2016) Wound healing efficacy
of a 660 nm diode laser in a rat incisional wound model. Lasers Med Sci 31:
1683-1689.
19. Mun S, Cheon M, Kim SH, Choi N, Kim S, et al.
(2013) The effect of laser diode irradiation on wound healing of rat skin. J
Cosmet Laser Ther 15: 318-325.
20. Paysse EA, Hussein MA, Miller AM, Brady McCreery
KM, Coats DK (2007) Pulsed mode versus near-continuous mode delivery of diode
laser photocoagulation for high-risk retinopathy of prematurity. J Aapos 11:
388-392.
21. Bryant GL, Davidson JM, Ossoff RH, Garrett CG,
Reinisch L (1998) Histologic study of oral mucosa wound healing: A comparison
of a 6.0-6.8 µm pulsed laser and a carbon dioxide laser. Laryngoscope 108:
13-17.
22. Havel M, Betz CS, Leunig A, Sroka R (2014) Diode
laser-induced tissue effects: In vitro tissue model study and in vivo
evaluation of wound healing following non-contact application. Lasers Surg Med
46: 449-455.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Advance Research on Alzheimers and Parkinsons Disease
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Allergy Research (ISSN:2642-326X)
- International Journal of Diabetes (ISSN: 2644-3031)